Introduction
The therapeutic anticoagulation of cancer-associated venous thromboembolism (VTE) is challenging because of the increased risk for thromboembolic recurrence and major bleeds (MB). Direct oral anticoagulants (DOACs) have emerged over Low Molecular Weight Heparin (LMWH) as a preferred treatment option by improving efficacy without compromising safety. Despite these advantages, major bleeding was noted to be a safety concern in recent randomized clinical trials, mainly for gastrointestinal (GI) and genitourinary (GU) high-risk cancer patients. We evaluated our cancer center's institutional experience to determine the safety signals among VTE treatments and clinical risk factors which can predict an adverse outcome to further develop our clinical practice decisions in oncology patients.
Methods
This is a retrospective chart review of patients receiving DOACs and LMWH with histologically proven GI or GU malignancy and symptomatic or incidental VTE treated at The University of Arizona Cancer Center from November 2013 to February 2020. Patients were excluded if DOACs were prescribed for any other reason not related to VTE, or the thrombotic event was determined to be unrelated to active malignancy. The primary safety outcome was defined as documented major bleeding by hemoglobin reduction of ≥2 g/dL, transfusion of ≥2 units of Packed Red Blood Cells, bleeding in a critical site, or bleeding contributing to death. The secondary efficacy outcome was defined as documented recurrent deep vein thrombosis (DVT), nonfatal pulmonary embolism (PE), or fatal PE. Data was collected as individually and composite outcome (MB+rVTE) before six months. Continuous non-normally distributed data are compared using the non-parametric Kruskal-Wallis Rank Sum. Categorical data are compared using χ2 or Fisher's exact test. Logistic regression was used to assess the relationship between anticoagulant therapy and the 3 outcome measurements. The relationship between therapies was adjusted for clinical risk factors using logistic regression. Statistical analyses were performed using Stata16.
Results
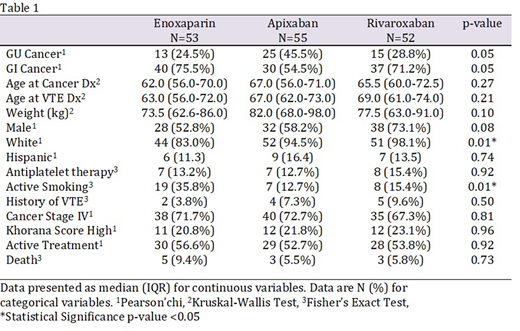
Our review included 160 patients with similar baseline characteristics who were prescribed enoxaparin (n=53), apixaban (n=55), and rivaroxaban (n=52) except for white race and active smokers [Table 1]. Primary MB outcome events at six months were 7.5%, 10.9%, and 17.3% for enoxaparin, apixaban, and rivaroxaban, with no statistical difference among therapies or cancer type [p>0.05]. Secondary rVTE outcome events at six months were 7.5%, 3.6%, and 5.7% for enoxaparin, apixaban, and rivaroxaban, respectively, with no significant difference among therapies or cancer type [p>0.05]. There were no differences in individual or composite outcomes of LMWH, apixaban, rivaroxaban, or DOAC by GI or GU cancer type. There are no statistically significant clinical associations between anticoagulation therapy by the three outcome measurements in either GI or GU cancer. Beyond six months on enoxaparin, apixaban, and rivaroxaban, there were 5.6%, 3.6%, and 5.7% added events to MB, and 3.7%, 1.8%, and 0% to rVTE, respectively.
Conclusions
Our retrospective review has shown similar efficacy in preventing recurrent VTE among anticoagulants and indirectly equivalent to those published by the randomized clinical trials. Notably, the rate of MB for our real-world high-risk GI/GU cancer was 2.8 times higher in patients receiving DOACs compared to those on clinical trial [MB 6% SELECT-D Young et al. 2018 and MB 3.8% Caravaggio Agnelli et al. 2020] and in agreement with a recent meta-analysis [relative risk GI 1.9 and GU 4.9, Giustozzi et al. 2020]. We recognized there are inherited selection bias in both clinical trials and retrospective studies, although baseline characteristics are similar. Future clinical trial designs should consider including real-world high-risk patients according to associated clinical risk factors to aid in the appropriate choice of therapeutic anticoagulation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.